Liver Diseases
Importance of Liver
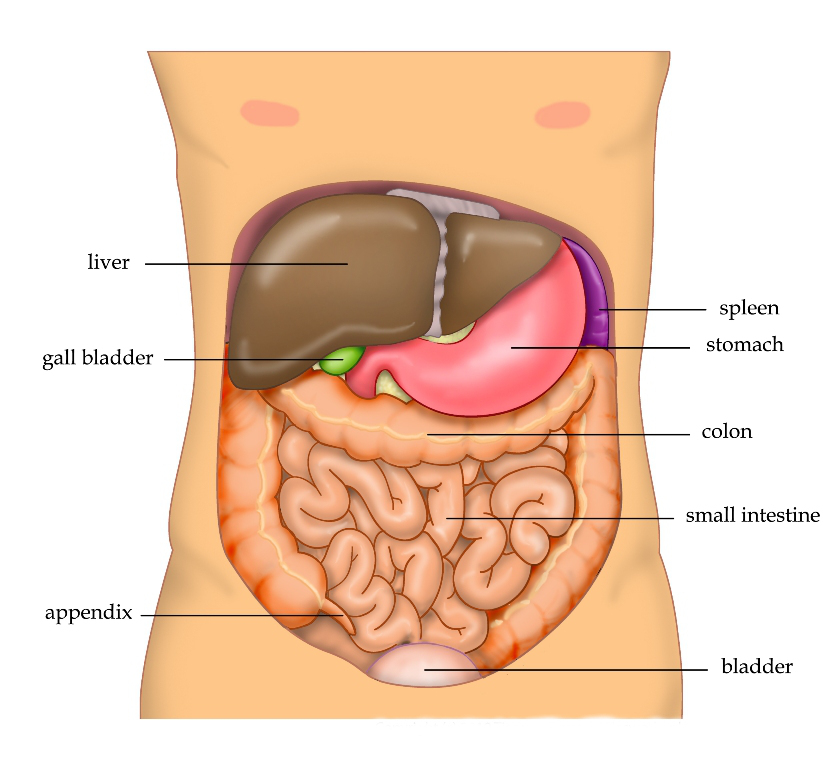
You can make do with only one kidney. You can survive without a spleen or a gallbladder. You can even get by without a stomach. But you can’t live without a liver, the body’s largest internal organ. It sits just under your ribcage on the right side and is about the size of a football. First and foremost, it plays the role of bouncer, keeping unwanted guests out of your bloodstream. Whatever you absorb through your digestive tract isn’t immediately circulated throughout your body. The blood from your intestines first goes straight to the liver, where nutrients are metabolized and toxins are neutralized.
Liver diseases
Liver cancer is rising 4 percent every year over the last decade. Liver dysfunction can run in families, like the iron-overload disease hemochromatosis. It can be caused by infections that can lead to liver cancer, or it can stem from drugs (most often overdoses of Tylenol). The most common causes are drink and food : alcoholic liver disease and fatty liver disease. Over time, liver disease can cause cirrhosis (scarring). As more scar tissue replaces healthy liver tissue, the liver can no longer function properly. Left untreated, liver disease can lead to liver failure and liver cancer. Early treatment can help heal the damage and prevent liver failure.
Various Causes of Liver Diseases
Different types of liver disease result from different causes. Liver disease may result from:
Viral Infections
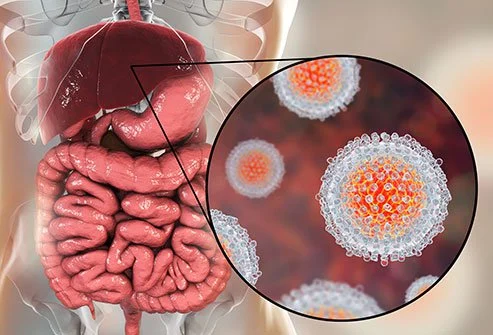
- Hepatitis A is spread primarily through food or water that is tainted with contaminated feces. It can be prevented through vaccination, avoiding raw and undercooked shellfish, and trying to ensure that everyone who handles your food washes their hands after changing nappies or using the toilet.
- Hepatitis B :- You get it from somebody else, such as through unprotected sex or taking drugs with shared needles. If it lasts longer than 6 months, it makes you more likely to get liver cancer or other diseases. Vaccination is available and given to every child.
- Hepatitis C is the most dreaded of liver viruses and no vaccine is available. Exposure can lead to a chronic infection that, over decades, can lead to cirrhosis and liver failure. This is now the leading cause of liver transplants. Hepatitis C is transmitted via blood, usually through sharing needles rather than via blood transfusion, now that the blood supply is screened for the virus.
- Hepatitis D virus infection can only occur in someone who is already infected with hepatitis B and so can be prevented by preventing hepatitis B. So get vaccinated and refrain from intravenous drug use and unsafe sex.
- Hepatitis E is considered a zoonotic disease, able to spread from animals to humans, and pigs may be the primary viral reservoir.
Immune System Problems
When your immune system mistakenly attacks your liver, it can cause autoimmune liver diseases. These include primary biliary cholangitis and autoimmune hepatitis.
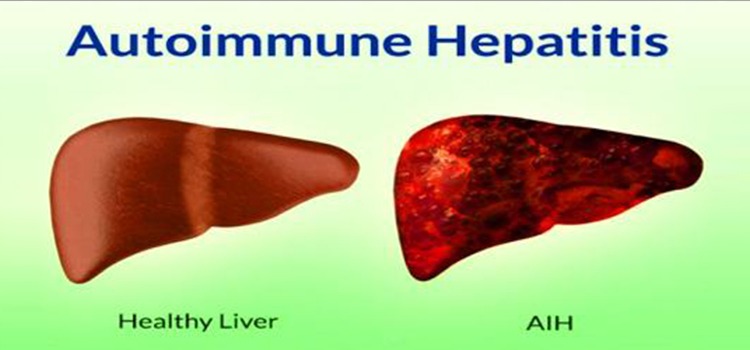
- Autoimmune hepatitis inflames your liver. It can lead to other disorders and even liver failure. It strikes girls and women more often than boys or men.
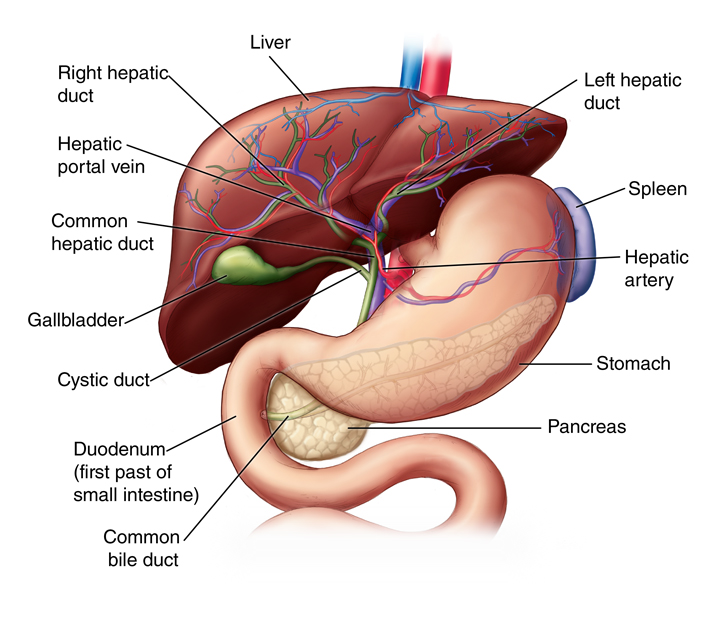
- Primary biliary cholangitis attacks tiny tubes in your liver called bile ducts. They carry bile, a chemical that helps you digest food. When the ducts are injured, the bile backs up inside your liver and scars it. Women come down with this more often than men.
- Primary sclerosing cholangitis scars your bile ducts, and it can eventually block them. The bile builds up inside your liver, and that makes it harder for your liver to work. It may lead to liver cancer, and you might someday need a liver transplant. Men are more likely than women to get it.
Inherited Diseases
Some liver problems develop because of a genetic condition (one you inherit from your parents). Inherited liver diseases include Wilson disease and hemochromatosis.
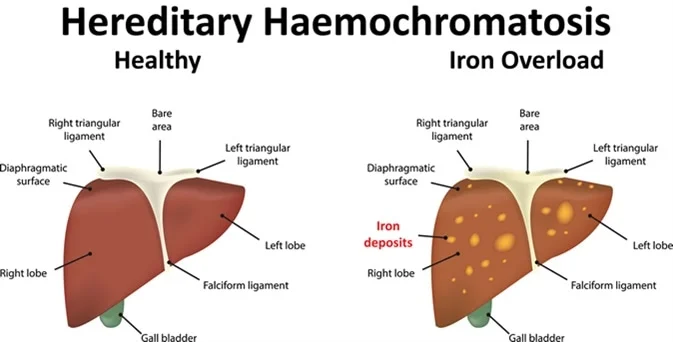
- Hemochromatosis makes your body store up too much of the iron from your food. The extra iron builds up in your liver, heart, or other organs. It can lead to life-threatening conditions such as liver diseases, heart disease, or diabetes.
- Hyperoxaluria hits when your urine has too much of a chemical called oxalate. In this condition, your liver makes too little much oxalate due to a genetic mutation. This can cause kidney stones and kidney failure. If your kidneys do fail, that can give you oxalosis, where the oxalate collects in other organs and causes more trouble.
- Wilson’s disease makes copper build up in your liver and other organs. Its first symptoms usually show up when you’re between the ages of 6 and 35, most often in your teens. It not only affects your liver, but it can cause nerve and psychiatric problems.
- Alpha-1 antitrypsin deficiency involves a chemical that helps your lungs resist infections. Your liver makes it. But when your liver gets the recipe wrong, the faulty chemical can build up and cause liver disease.
Cancer and Tumors
If cancer shows up in your liver, that’s most likely because it has spread from another part of your body, like your lungs, colon, or breasts. But a few cancers can start in the liver.
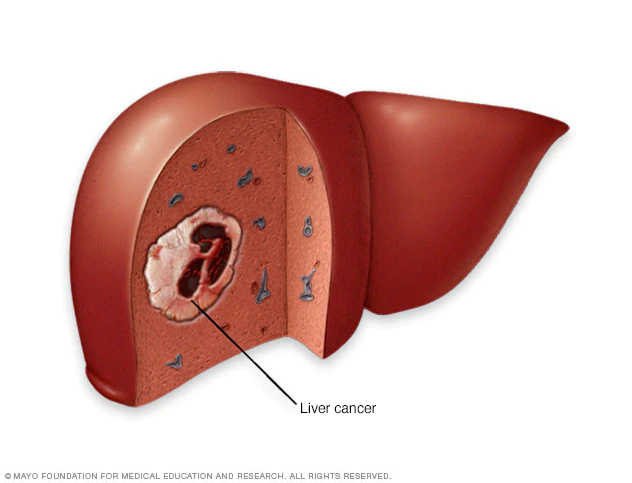
- Liver cancer affects women more often than men, and African-Americans more often than whites. Your doctor might call it hepatocellular carcinoma. It’s more likely if you have hepatitis or drink too much.
- Bile duct cancer strikes the tubes that run from your liver to your small intestine to carry bile, a fluid that helps you digest food. This kind of cancer mainly affects people over age 50, but it’s uncommon.
- Liver cell adenoma is a tumor that doesn’t have cancer. It’s uncommon, but women who take birth control pills for a long time are more prone than other people to develop it. There’s a small chance the tumor could eventually turn into cancer.
Other Causes
Alcoholic fatty liver disease is the result of misusing alcohol. Nonalcoholic fatty liver disease (NAFLD) results from consuming too much fat. NAFLD is becoming more common as rates of obesity and diabetes rise.
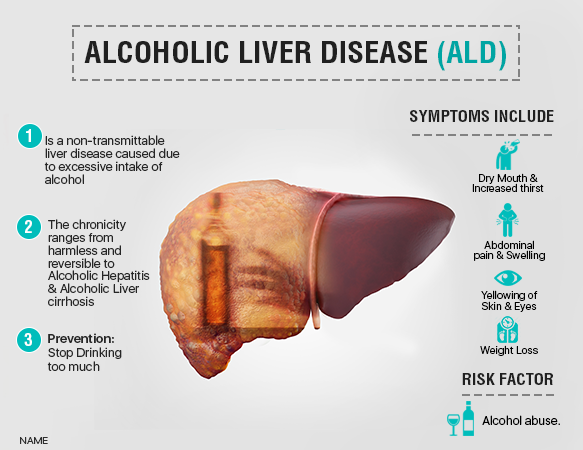
- Alcoholic liver disease :- Excessive alcohol consumption can lead to an accumulation of fat in the liver (fatty liver), which can cause inflammation and result in liver scarring and eventually liver failure. Heavy alcohol consumption can cause a fatty liver in less than three weeks, but it usually resolved within 4-6 weeks after stopping drinking. But in 5-15% cases, the disease continue to progress and the liver starts to scar despite alcohol cessation.
- Once alcohol-induced hepatitis (liver inflammation) is diagnosed, three year survival rates can be as high as 90 percent among people who stop drinking after diagnosis. But as many as 18 percent of them go on to develop cirrhosis, an irreparable scarring of the liver.
- The CDC defines excessive drinking as the regular consumption of more than one drink a day for women and more than two a day for men. A drink is defined as 12 ounces of beer, 8 ounces of high alcohol beer, 5 ounces of wine, or 1.5 ouncess of spirits.
- Drug overdoses. Taking too much acetaminophen or other medications can harm your liver. Make sure you follow the dosing instructions on the label, and be aware that acetaminophen might be in more than one medicine you take.
- Non-alcoholic liver disease :- Characterised as a “tale of fat and sugar” but not all fat affects the liver similarly. People suffering from fatty liver inflammation were found to be consuming more animal fat (and cholesterol) but less plant fat (and fibre and antioxidants). It can also be caused by cholesterol overload. The dietary cholesterol found in eggs, meat and dairy can become oxidized and then set off a chain reaction that results in excess fat in the liver. When the concentration of cholesterol in your liver cells get too high, it can crystallize like a stick of rock and result in inflammation. Your WBCs try to engulf the cholesterol crystals but then die in the process, spilling out inflammatory compounds. Best way to avoid live diseases is to avoid excess calories, cholesterol, saturated fat and sugar.
Dire complications of liver disease include:
- Acute liver failure. This happens when you don’t have a long-term liver disease but your liver quits working within a very short time — days or weeks. That may happen because of an overdose of acetaminophen, infections, or because of prescription drugs.
- Cirrhosisis a buildup of scars in your liver. The more scars replace the healthy parts of your liver, the harder it is for your liver to do its job. Over time, it may not work like it should.
Symptoms of liver disease
Some types of liver disease (including nonalcoholic fatty liver disease) rarely cause symptoms. For other conditions, the most common symptom is jaundice — a yellowing of your skin and the whites of your eyes. Jaundice develops when your liver can’t clear a substance called bilirubin.

Other signs of liver disease may include:
- Abdominal (belly) pain (especially on the right side).
- Bruising easily.
- Changes in the color of your urine or stool.
- Fatigue.
- Nausea or vomiting.
- Swelling in your arms or legs (edema).
How is liver disease diagnosed ?
To accurately diagnose and find the cause of liver disease, your provider will also recommend one or more tests. These may include:
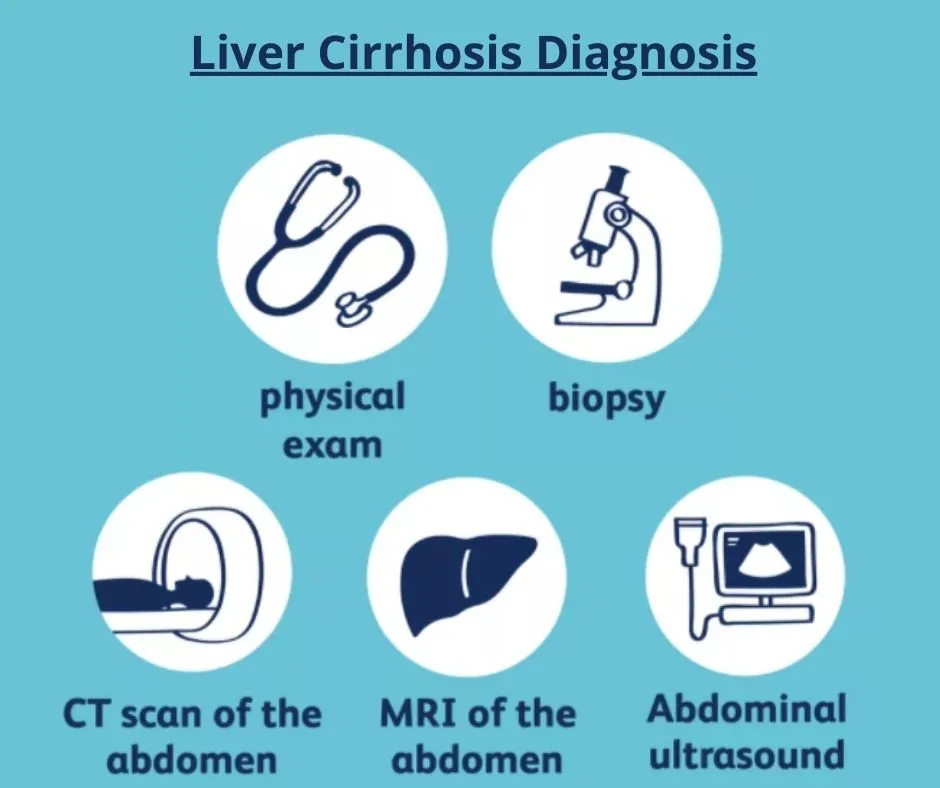
- Blood tests: Liver enzymes measure levels of liver enzymes in your blood. Other tests of liver function include a blood-clotting test called the international normalized ratio (INR). Abnormal levels may indicate problems with your liver function.
- Imaging tests: Your provider can use ultrasound, MRI or CT scan to look for signs of damage, scarring or tumors in your liver. Another specialized type of ultrasound called fibroscan can be used to determine the degree of scarring and fat deposition in the liver.
- Liver biopsy: During a liver biopsy, your provider uses a thin needle to remove a small sample of liver tissue. They analyze the tissue to look for signs of liver disease.
How is liver disease managed or treated ?
Treatment for liver disease depends on the type of liver disease you have and how far it has progressed. Possible treatments include:
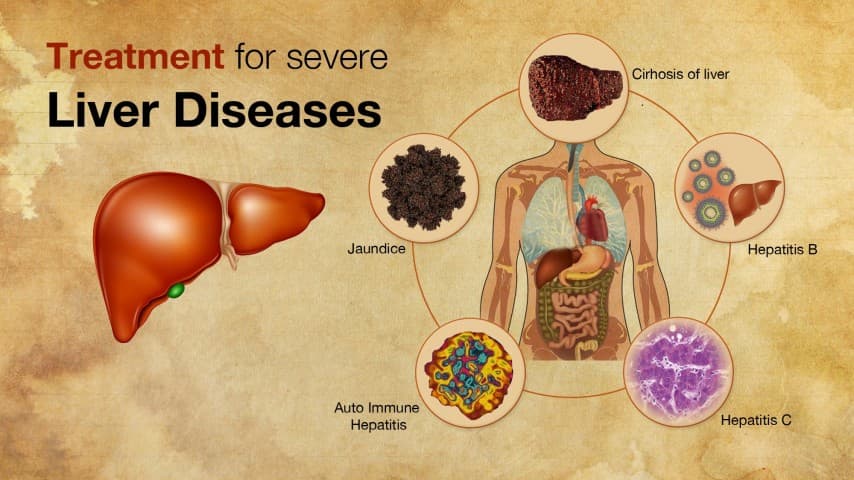
- Medications: Healthcare providers treat some types of liver disease with medication. You may take medicine for viral infections like hepatitis or inherited conditions like Wilson disease.
- Lifestyle changes: You can use your diet to help manage certain types of liver disease. If you have fatty liver disease, avoiding alcohol, limiting fat and calories and increasing fiber intake can help. Alcohol-related liver disease can improve with abstinence from alcohol.
- Liver transplant: When liver disease progresses to liver failure, a liver transplant may be the best treatment option. A transplant replaces your liver with a healthy liver.
Can liver diseases be prevented?
You can take steps to prevent some types of liver disease — especially those affected by your diet and lifestyle. If you are at risk for liver disease, your provider may recommend lifestyle changes including:
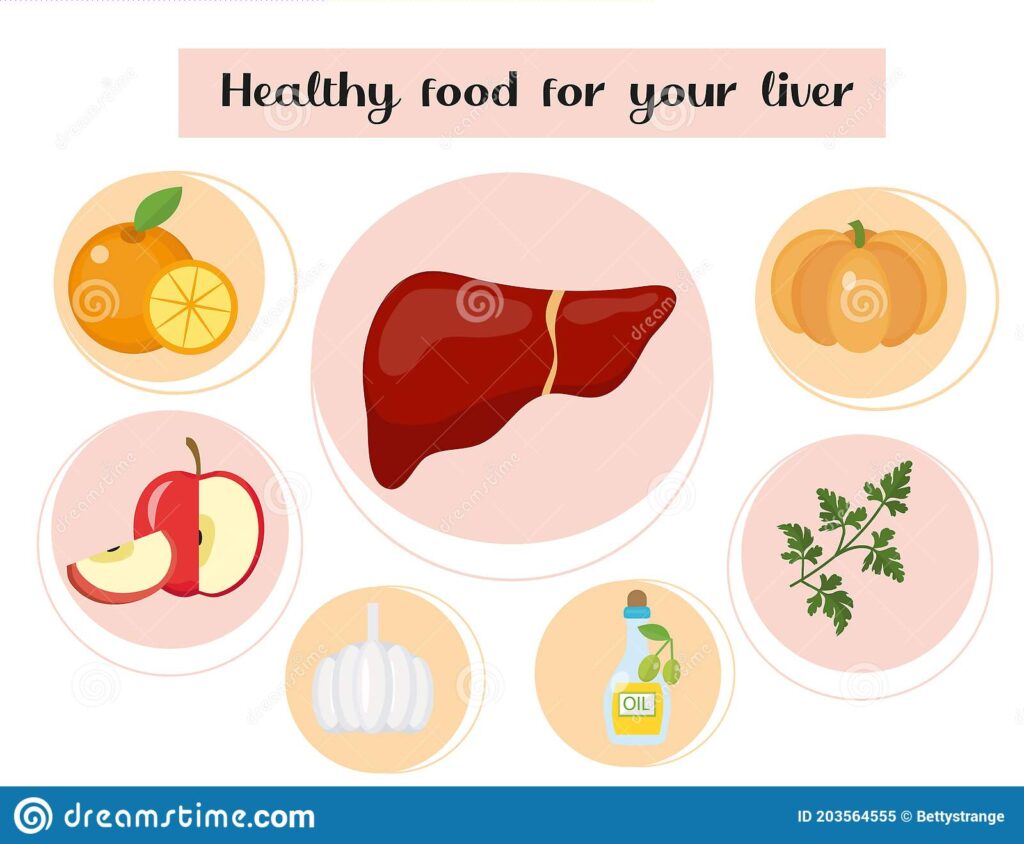
- Avoiding or limiting alcohol.
- Avoiding foods and drinks that contain trans fats or high-fructose corn syrup.
- Carefully managing your intake of prescription and over-the-counter medications to avoid liver damage, as medications like acetaminophen (Tylenol®) are a common cause of liver injury.
- Getting regular exercise.
- Limiting consumption of red meat.
- Oatmeal can reduce inflammation and also weight.
- Consumption of four or more cups of coffee a day was associated with 92% lower risk among smokers dying from chronic liver disease. Coffee consumption may reduce DNA damage, increase the clearance if virus infected cells and slow the scarring process.
You can minimize the likelihood of contracting viral hepatitis by practicing safe sex and not sharing needles.